Medicare Part B 2026: 10% Premium Adjustments Explained

Medicare Part B premiums for 2026 could see potential 10% adjustments, influenced by healthcare spending, inflation, and legislative decisions, directly impacting beneficiaries’ out-of-pocket costs and financial planning.
The landscape of healthcare costs is constantly evolving, and for millions of Americans, understanding these shifts is paramount to financial well-being. The anticipated New Medicare Part B Changes for 2026: A Detailed Look at Potential 10% Premium Adjustments are particularly significant, signaling a potential increase that could affect how beneficiaries plan their future healthcare expenses.
Understanding Medicare Part B and Its Importance
Medicare Part B is a cornerstone of healthcare coverage for millions of Americans, primarily covering medically necessary services and preventive care. This includes doctor visits, outpatient hospital care, mental health services, and various medical equipment. Its comprehensive nature makes it an indispensable component of the broader Medicare program, ensuring beneficiaries have access to essential medical attention that extends beyond inpatient hospital stays.
For many, Part B is the primary means of accessing routine medical care, making its premium structure a critical point of interest. The premiums are typically deducted directly from Social Security benefits, or beneficiaries receive a bill from Medicare. Understanding what Part B covers and how its costs are determined is the first step in preparing for any future adjustments.
What Medicare Part B Covers
Medicare Part B specifically targets services that are medically necessary to treat a disease or condition, as well as preventive services to keep you healthy. This includes a wide array of healthcare provisions:
- Doctor services, including those provided in an office or other outpatient setting.
- Outpatient care, such as emergency room visits or observation stays that do not lead to an inpatient admission.
- Preventive services, including screenings, shots, and certain health education programs designed to prevent illness.
- Durable medical equipment (DME), like wheelchairs, walkers, and oxygen equipment.
These coverages are vital for maintaining health and managing chronic conditions, highlighting why changes to its premium structure can have a profound impact on beneficiaries’ budgets.
How Premiums are Determined
Medicare Part B premiums are not static; they are assessed annually and can change based on several factors. The Centers for Medicare & Medicaid Services (CMS) is responsible for setting these premiums. Key determinants include:
- The cost of healthcare services utilized by beneficiaries.
- The overall financial health of the Medicare program.
- Legislative actions and policy changes.
- Income-related monthly adjustment amounts (IRMAA) for higher-income beneficiaries.
These elements combine to project the necessary funding for Part B services, ultimately influencing the premium amounts. The anticipation of a 10% adjustment for 2026 suggests that these underlying factors are signaling a need for increased revenue to sustain the program’s offerings.
In essence, Medicare Part B provides a critical safety net for medical expenses outside of hospital stays. Its premiums, while subject to annual review, reflect the ongoing costs of delivering these essential healthcare services to an aging population.
Factors Driving the Potential 10% Premium Adjustments
The projection of a potential 10% premium adjustment for Medicare Part B in 2026 is not an arbitrary figure; it stems from a complex interplay of economic and healthcare-specific factors. Understanding these drivers is crucial for beneficiaries to grasp the rationale behind such significant changes and to plan accordingly.
Several key elements contribute to the rising costs within the healthcare system, which in turn place upward pressure on Medicare Part B premiums. These factors often interact, creating a cumulative effect that necessitates adjustments to maintain the program’s solvency and coverage levels.
Rising Healthcare Utilization and Costs
One of the primary drivers is the escalating cost of healthcare services and the increasing utilization of these services. As the population ages, more individuals require medical attention, leading to higher demand for doctor visits, specialized treatments, and prescription drugs. The development of new, often more expensive medical technologies and treatments also contributes to this upward trend.
Furthermore, the cost of labor within the healthcare sector, including salaries for doctors, nurses, and support staff, continues to rise. These operational expenses are inevitably passed on, in part, to programs like Medicare, influencing premium calculations.
Inflationary Pressures
Inflation, a broad economic phenomenon, significantly impacts healthcare costs. When the cost of goods and services across the economy rises, healthcare is not immune. The prices of medical supplies, equipment, and pharmaceuticals increase, directly affecting the expenses incurred by Medicare Part B. High inflation rates can erode the purchasing power of the Medicare trust fund, necessitating higher premiums to cover the same level of services.
The economic environment leading up to 2026, including global supply chain issues and fiscal policies, will play a substantial role in determining the extent of inflationary pressure on healthcare expenditures.
Legislative and Policy Decisions
Government policies and legislative decisions also exert considerable influence on Medicare Part B premiums. Changes to healthcare laws, adjustments to reimbursement rates for providers, and new mandates for covered services can all alter the financial landscape of the program. For instance, decisions regarding prescription drug pricing or the expansion of certain preventive services can directly impact the overall cost structure.
Future legislative actions leading up to 2026 could introduce new variables that either mitigate or exacerbate the need for premium adjustments. These decisions are often the result of extensive debate and negotiation within Congress, reflecting broader societal priorities and economic realities.
In summary, the confluence of increased healthcare utilization, persistent inflationary pressures, and strategic legislative decisions are the main forces behind the projected 10% premium adjustments for Medicare Part B in 2026. These factors underscore the dynamic nature of healthcare finance and the continuous need for careful financial planning among beneficiaries.
Historical Context of Medicare Part B Premium Increases
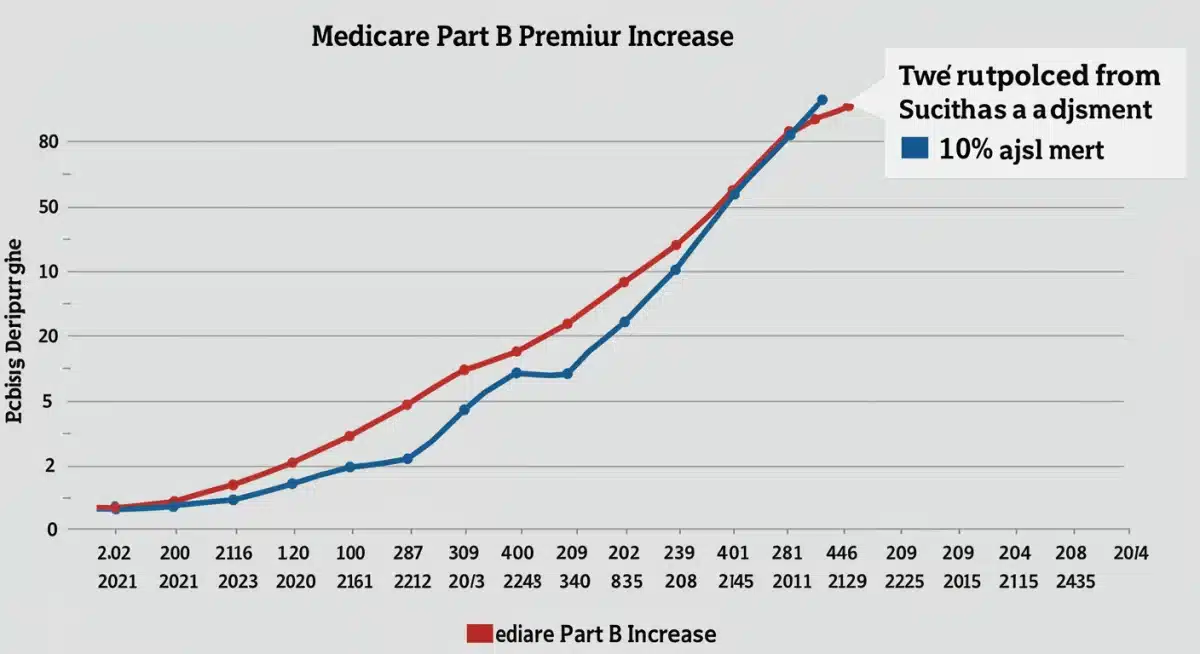
To fully appreciate the significance of a potential 10% increase in Medicare Part B premiums for 2026, it’s beneficial to look back at historical trends. Medicare premiums have rarely remained static, reflecting the ever-changing economic and healthcare landscape. Examining past adjustments can provide valuable insights into the patterns and underlying reasons for such changes.
Over the years, beneficiaries have experienced a range of premium adjustments, from modest increases to more substantial hikes. These changes are typically announced in the fall of the preceding year, giving beneficiaries some time to prepare. The historical data reveal that various factors, including medical advancements, economic downturns, and legislative reforms, have all played a role in shaping premium costs.
Previous Significant Premium Increases
There have been several periods where Medicare Part B premiums saw notable increases. For example, in years following major healthcare legislation or significant upticks in medical inflation, premiums have often climbed. These increases are generally necessary to ensure the solvency of the program and to cover the rising costs of providing comprehensive medical services.
One particularly memorable increase occurred in 2016, where a select group of beneficiaries faced a substantial premium hike due to a provision in the law. While not a universal increase, it highlighted how specific legislative acts could disproportionately affect certain groups. Understanding these precedents helps contextualize the current projections.
Impact of Economic Fluctuations
Economic conditions have a direct bearing on Medicare Part B premiums. During periods of economic growth and low unemployment, the tax revenues supporting Medicare tend to be more robust. Conversely, economic downturns can strain the system, potentially leading to higher premiums to offset shortfalls.
Inflationary periods, as discussed earlier, also contribute significantly. When the cost of living rises, so too do the costs associated with healthcare delivery, from medical supplies to personnel wages. These macroeconomic factors are consistently evaluated by CMS when determining annual premium adjustments.
Legislative Reforms and Their Effects
Major legislative reforms, such as the Affordable Care Act (ACA), have also had long-term impacts on Medicare Part B. While not always directly leading to immediate premium increases, these reforms can alter the structure of healthcare delivery and financing, which eventually influences the program’s costs. For instance, mandates for certain preventive services or changes to physician reimbursement schedules can shift financial burdens.
Looking at the historical context, it’s clear that Medicare Part B premiums are a dynamic reflection of broader economic health, medical innovation, and legislative priorities. The projected 10% increase for 2026 is therefore part of an ongoing pattern of adjustments designed to keep the program viable and responsive to the healthcare needs of its beneficiaries.
Potential Impact on Beneficiaries and Financial Planning
A potential 10% increase in Medicare Part B premiums for 2026 could have significant ramifications for beneficiaries, particularly those on fixed incomes. Understanding these potential impacts and proactively engaging in financial planning is crucial to mitigating the effects of such an adjustment.
For many, Medicare premiums represent a substantial portion of their monthly expenditures. An increase, even if seemingly modest in percentage, can translate into a notable reduction in disposable income, affecting daily living expenses, savings, and overall financial stability. It’s not just about the premium itself, but how it interacts with other healthcare costs and personal budgets.
Budgetary Considerations for Seniors
Many seniors rely on Social Security benefits as their primary source of income. Since Medicare Part B premiums are often deducted directly from these benefits, an increase effectively reduces their net Social Security payment. This can strain budgets already stretched thin by rising costs of living, including housing, food, and other utilities.
Beneficiaries will need to re-evaluate their monthly budgets to accommodate this potential increase. This might involve adjusting spending habits, revisiting retirement savings plans, or exploring additional income streams if feasible. The goal is to ensure that essential needs can still be met without undue financial stress.
Strategies for Mitigating the Impact
There are several proactive steps beneficiaries can take to prepare for and potentially mitigate the impact of higher premiums. Financial planning should begin well in advance of the 2026 changes.
- Reviewing Income and Expenses: A comprehensive review of current income and expenditures can identify areas where adjustments can be made.
- Exploring Medicare Advantage Plans: Some Medicare Advantage plans (Part C) offer lower Part B premiums or even rebate a portion of the premium, though they come with their own network restrictions and cost-sharing structures.
- Medigap Policies: For those with Medigap plans, understanding how premium increases might interact with their supplemental coverage is important. While Medigap doesn’t cover Part B premiums, it can help with other out-of-pocket costs, potentially freeing up funds for higher premiums.
- State Assistance Programs: Low-income beneficiaries may qualify for state-run Medicare Savings Programs (MSPs), which can help pay for Part B premiums, deductibles, and co-insurance.
These strategies offer avenues for beneficiaries to take control of their financial health in the face of impending changes. Early planning and exploration of available resources are key.
Long-Term Financial Planning
Beyond immediate adjustments, the potential 10% increase highlights the importance of long-term financial planning for retirement and healthcare costs. Future premium increases are always a possibility, and incorporating these potential fluctuations into long-term financial models can help ensure greater financial security.
Consulting with financial advisors who specialize in retirement planning and Medicare can provide personalized guidance, helping beneficiaries create robust financial strategies that account for evolving healthcare expenses. The aim is to build resilience against future cost adjustments, safeguarding financial well-being throughout retirement.
The Role of CMS and Congressional Oversight
The determination of Medicare Part B premiums is a complex process primarily overseen by the Centers for Medicare & Medicaid Services (CMS), with significant influence from congressional oversight and legislative mandates. Understanding the roles of these entities is crucial for comprehending how premium adjustments, such as the potential 10% increase for 2026, come into being.
CMS is the federal agency responsible for administering Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP). Among its many duties, CMS is tasked with setting the annual Part B premiums, a decision that balances the financial solvency of the program with the affordability for beneficiaries. This involves extensive data analysis, actuarial projections, and consideration of economic forecasts.
CMS’s Premium Setting Process
Each year, CMS actuaries analyze projected healthcare spending, trends in utilization, and the financial status of the Medicare Part B trust fund. They consider factors such as:
- Expected growth in healthcare costs, including physician services, outpatient care, and durable medical equipment.
- The impact of new medical technologies and prescription drugs.
- The number of eligible beneficiaries and their health status.
- Any legislative changes that affect Medicare’s financial structure.
Based on these projections, CMS proposes the standard monthly premium for the upcoming year. This process is designed to ensure that the premiums cover approximately 25% of the program’s costs, with general revenue funding the remaining 75%.
Congressional Influence and Legislative Mandates
While CMS sets the premiums, Congress plays a critical oversight role and can enact legislation that directly impacts the premium calculation. Lawmakers often deliberate on policies that aim to control healthcare costs, expand benefits, or provide financial relief to beneficiaries. These legislative mandates can either constrain or necessitate premium adjustments.
For example, the “hold harmless” provision, which prevents most beneficiaries from seeing their Part B premium increase by more than their Social Security cost-of-living adjustment (COLA), is a legislative protection. However, this provision doesn’t apply to all beneficiaries, particularly those new to Medicare, those who don’t receive Social Security benefits, or higher-income individuals subject to IRMAA.
Congressional hearings and debates also serve to scrutinize CMS’s projections and decisions, ensuring accountability and transparency in the premium-setting process. Political considerations, public pressure, and advocacy groups often weigh in, influencing the final outcomes.
Balancing Affordability and Program Solvency
The ongoing challenge for both CMS and Congress is to strike a delicate balance between making Medicare Part B affordable for beneficiaries and ensuring the long-term financial solvency of the program. Premium adjustments are a direct reflection of this balancing act. A 10% increase for 2026 suggests that the projected costs of maintaining the current level of services are rising significantly, requiring an upward adjustment to sustain the program.
The decisions made by CMS and the legislative actions taken by Congress are therefore pivotal in shaping the future of Medicare Part B, directly impacting the financial well-being of millions of Americans reliant on its coverage.
Alternatives and Policy Discussions for Future Stability
The prospect of a 10% increase in Medicare Part B premiums for 2026 naturally sparks discussions about alternatives and policy solutions aimed at ensuring the program’s long-term stability and affordability. Policymakers, healthcare experts, and advocacy groups are continually exploring various strategies to manage costs without unduly burdening beneficiaries.
These discussions often revolve around systemic reforms, cost-containment measures, and innovative financing models. The goal is to create a sustainable Medicare system that can adapt to changing demographics, medical advancements, and economic realities while remaining accessible to all eligible Americans.
Cost-Containment Strategies
One major area of focus is implementing more effective cost-containment strategies within the healthcare system. This includes initiatives to reduce waste, fraud, and abuse, which divert significant resources from the program. Additionally, promoting value-based care models, where providers are incentivized for patient outcomes rather than the volume of services, can help control expenditures.
- Negotiating Drug Prices: Allowing Medicare to directly negotiate prescription drug prices, similar to practices in other countries, is a frequently debated proposal that could yield substantial savings.
- Promoting Preventive Care: Investing more in preventive services can reduce the incidence of chronic diseases and the need for more expensive acute care interventions down the line.
- Streamlining Administrative Processes: Reducing administrative overhead for both providers and the program can free up resources.
These measures aim to address the root causes of rising healthcare costs, thereby alleviating pressure on premiums.
Alternative Financing Models
Beyond cost control, discussions also include exploring alternative financing models for Medicare Part B. The current model, where premiums cover 25% and general revenues cover 75%, is subject to demographic and economic shifts. Some proposals suggest adjusting these proportions or introducing new revenue streams.
For instance, some economists advocate for broader tax reforms that could bolster Medicare’s financial standing, reducing the reliance on direct premium increases. Others suggest exploring means-testing adjustments that more finely tune premiums based on an individual’s financial capacity, beyond the current IRMAA thresholds.
Impact of Technological Advancements
Technological advancements, while often contributing to higher initial costs, also offer potential solutions for long-term stability. Telemedicine, for example, can reduce the need for expensive in-person visits and improve access to care, particularly in rural areas. Artificial intelligence and data analytics can enhance efficiency in claims processing and identify areas for cost savings.
However, careful management is required to ensure that technological integration does not inadvertently create new cost burdens or exacerbate existing disparities in access to care. The focus must be on leveraging technology to deliver more efficient, effective, and affordable healthcare.
Ultimately, the discussion surrounding Medicare Part B’s future stability is multifaceted, requiring a collaborative approach from policymakers, healthcare providers, and beneficiaries. By exploring and implementing a combination of cost-containment strategies, innovative financing, and technological integration, the aim is to ensure that Medicare Part B remains a robust and affordable program for generations to come, even in the face of potential premium adjustments like those projected for 2026.
Preparing for the 2026 Adjustments: Practical Advice
With the potential for a 10% increase in Medicare Part B premiums in 2026, proactive preparation is essential for beneficiaries. While the official announcement will come later, understanding practical steps now can help cushion the financial impact. This involves reviewing current coverage, assessing financial resources, and exploring all available options to optimize healthcare spending.
The goal is not just to react to the changes but to strategically plan ahead, ensuring that healthcare remains accessible and affordable without compromising other essential financial goals. This preparedness can alleviate stress and provide a sense of control over one’s healthcare future.
Reviewing Your Current Medicare Coverage
The first step is to thoroughly review your current Medicare coverage. Understand what your Part B covers, what your current premium is, and how it’s paid. If you have a Medicare Advantage plan (Part C) or a Medigap policy, examine how these interact with Part B and what changes they might undergo in conjunction with premium adjustments.
- Annual Enrollment Period: Be aware of the annual Medicare Open Enrollment Period (typically October 15th to December 7th) as an opportunity to change plans if a different option becomes more financially viable.
- Part D Coverage: If you have a standalone Part D prescription drug plan, assess its costs and coverage as well, as overall healthcare expenses are interconnected.
- Provider Networks: If considering a Medicare Advantage plan, ensure your preferred doctors and hospitals are within the plan’s network.
A comprehensive understanding of your existing coverage is the foundation for making informed decisions about future adjustments.
Assessing Your Financial Situation
Next, take a realistic look at your financial situation. Calculate your current monthly income and expenses, paying close attention to how much of your budget is allocated to healthcare. Consider how a 10% increase in Part B premiums would affect your disposable income.
If you anticipate financial strain, start exploring ways to adjust your budget now. This could involve cutting back on non-essential spending, looking for ways to reduce other fixed costs, or identifying potential sources of additional income. The earlier you identify potential gaps, the more time you have to address them.
Seeking Professional Guidance and Resources
Don’t hesitate to seek professional guidance. Financial advisors specializing in retirement planning can offer tailored advice on how to integrate potential Medicare cost increases into your overall financial strategy. They can help you explore investment strategies, savings plans, and other financial tools to build resilience against rising costs.
Additionally, state and federal resources are available to help beneficiaries navigate Medicare. State Health Insurance Assistance Programs (SHIPs) offer free, unbiased counseling on Medicare-related questions. Websites like Medicare.gov provide a wealth of information on different plans, eligibility, and financial assistance programs like Medicare Savings Programs (MSPs).
By actively reviewing coverage, assessing finances, and utilizing available resources, beneficiaries can effectively prepare for the New Medicare Part B Changes for 2026: A Detailed Look at Potential 10% Premium Adjustments. Proactive planning is the most effective way to maintain financial stability and ensure continued access to quality healthcare.
Long-Term Outlook for Medicare Part B Premiums
While the immediate focus is on the potential 10% premium adjustments for Medicare Part B in 2026, it’s equally important to consider the long-term outlook for the program’s costs and sustainability. Medicare is a dynamic system, constantly influenced by demographic shifts, medical advancements, and economic pressures. Understanding these broader trends can help beneficiaries and policymakers anticipate future challenges and plan accordingly.
The trajectory of healthcare costs in the United States suggests that upward pressure on premiums is likely to continue for the foreseeable future, absent significant systemic reforms. The aging of the baby boomer generation, coupled with continuous innovation in medical treatments, means that the demand for and cost of healthcare services will remain high.
Demographic Shifts and Increased Demand
The aging population is a primary driver of long-term Medicare costs. As more Americans enter retirement and live longer, healthier lives, they will rely on Medicare for a greater duration. This demographic shift leads to an increased number of beneficiaries, which naturally translates to higher overall program expenditures. The ratio of workers contributing to Medicare to retirees receiving benefits is also shifting, placing greater strain on the system.
This increased demand necessitates a robust funding mechanism, and premiums are one component of that. Without substantial changes to how healthcare is delivered or financed, the demographic trends alone suggest a continued need for periodic premium adjustments.
Innovation and Medical Advancements
Medical innovation, while a boon for public health, often comes at a high cost. New diagnostic tools, advanced surgical techniques, and groundbreaking pharmaceutical treatments can significantly improve patient outcomes but also add to the overall expense of healthcare. Medicare, by design, strives to cover medically necessary and effective treatments, which means it must absorb the costs associated with these advancements.
While some innovations may eventually lead to cost savings through more efficient care, the initial introduction of new technologies and therapies typically drives up expenses. This presents a perpetual challenge for Medicare, balancing access to cutting-edge care with financial sustainability.
Policy Debates and Future Reforms
The long-term outlook for Medicare Part B premiums will also be shaped by ongoing policy debates and potential future reforms. Discussions about the solvency of the Medicare trust funds are a recurring theme in Washington, D.C. Various proposals are continually put forth, ranging from adjustments to eligibility ages, changes to cost-sharing structures, to reforms in how providers are reimbursed.
Future legislative actions, potentially driven by economic conditions or political priorities, could introduce structural changes to Medicare Part B that impact premiums. These could include measures to further control drug prices, promote greater competition among providers, or re-evaluate the income-related monthly adjustment amounts (IRMAA) thresholds.
In conclusion, while the potential 10% increase for 2026 is a near-term concern, beneficiaries and policymakers alike must maintain a long-term perspective on Medicare Part B premiums. The interplay of demographic shifts, medical innovation, and ongoing policy debates will continue to influence the program’s financial requirements, making informed planning and adaptive strategies essential for future stability.
| Key Aspect | Brief Description |
|---|---|
| Potential 10% Increase | Medicare Part B premiums for 2026 are projected to increase by up to 10%, impacting monthly healthcare costs for beneficiaries. |
| Driving Factors | Key drivers include rising healthcare utilization, general inflation, and legislative decisions affecting Medicare’s financial structure. |
| Beneficiary Impact | Increased premiums will necessitate budget re-evaluation, potential adjustments to financial planning, and exploration of assistance programs. |
| Preparation Strategies | Review current coverage, assess personal finances, and consider consulting financial advisors or SHIPs for guidance. |
Frequently Asked Questions About 2026 Medicare Part B Changes
Medicare Part B is medical insurance covering medically necessary services like doctor visits, outpatient care, and preventive services. It also includes durable medical equipment and some mental health services, acting as a crucial component of overall Medicare coverage for millions of Americans.
The potential 10% increase for 2026 is driven by several factors, including rising healthcare utilization, general economic inflation impacting medical costs, and various legislative or policy decisions affecting Medicare’s financial structure and reimbursement rates for providers.
A 10% premium increase will directly reduce your net Social Security benefits if premiums are deducted automatically. This requires beneficiaries, especially those on fixed incomes, to re-evaluate their monthly budgets and potentially adjust spending or seek additional financial assistance to cover the increased cost.
To prepare, review your current Medicare coverage, assess your financial situation, and explore options like Medicare Advantage plans, Medigap policies, or state assistance programs. Consulting a financial advisor or SHIP counselor can also provide personalized guidance and strategies for managing costs.
The Centers for Medicare & Medicaid Services (CMS) is primarily responsible for setting Medicare Part B premiums annually. These decisions are made in consultation with actuarial projections and are subject to congressional oversight and legislative mandates that balance program solvency with beneficiary affordability.
Conclusion
The anticipated New Medicare Part B Changes for 2026: A Detailed Look at Potential 10% Premium Adjustments underscore the dynamic nature of healthcare financing in the United States. While the prospect of increased costs can be daunting, understanding the underlying factors and taking proactive steps can significantly mitigate the financial impact on beneficiaries. By staying informed, meticulously reviewing personal finances, and leveraging available resources and professional guidance, individuals can navigate these changes effectively, ensuring continued access to essential healthcare services without compromising their financial well-being. The ongoing dialogue among policymakers about long-term stability and affordability remains crucial for the future of Medicare Part B.





